As we age, how we care for and maintain our teeth changes. Chewing and biting can become painful, making eating difficult. This leads to nutritional deficiencies, jawbone loss, and decreased self-confidence. Dental implants for seniors are becoming a popular solution to address these issues and maintain a healthy smile even in the golden years.
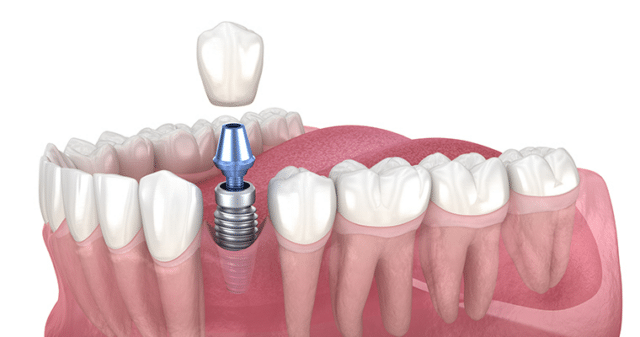
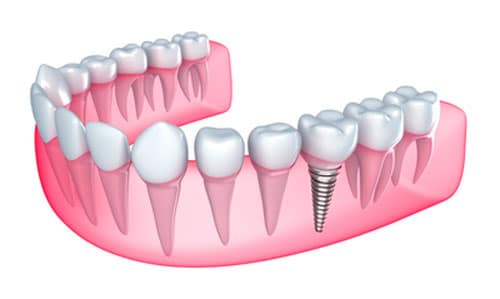
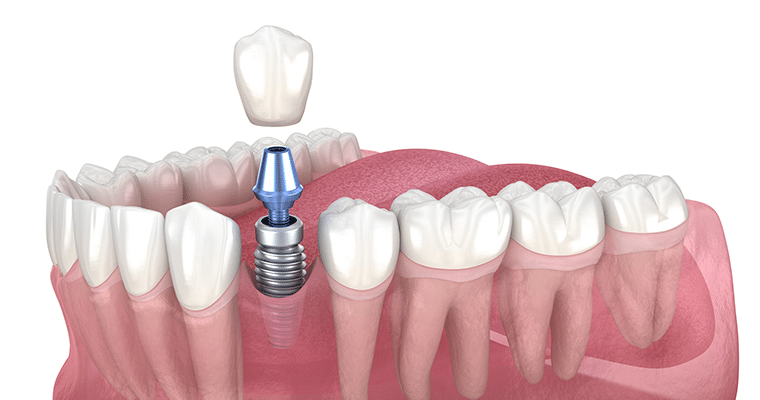
Dental implants are artificial tooth roots placed into the jawbone to support dental prosthetics. They have gained popularity due to their natural appearance and ability to restore full functionality to the mouth. This is particularly important for older adults, as maintaining good dental health is crucial for overall well-being and quality of life.
This blog explores implant dentistry for older adults, guiding you to help you make informed decisions about your dental health and determine if dental implants for seniors are the right option for you.

Benefits of Implant Dentistry for Older Adults
The following are the most notable benefits of dental implants for seniors:
Improved Facial Appearance and Bone Preservation
Dental implants for seniors offer a significant facial appearance and bone preservation advantage. As we age, tooth loss can lead to a sunken facial structure due to bone loss in the jaw. Dental implants provide the necessary stimulation to the jawbone, helping to maintain its density and shape. This preserves a more youthful facial appearance and supports overall oral health.
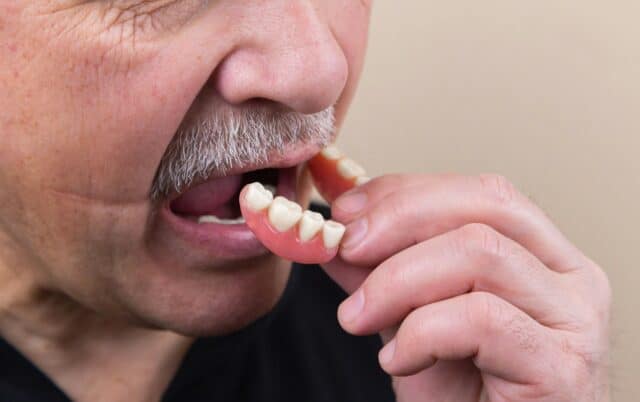
Enhanced Comfort and Stability Compared to Traditional Dentures
One of the primary benefits of dental implants for seniors is the enhanced comfort and stability they provide. Unlike traditional dentures, which can slip and cause discomfort, dental implants are securely attached to the jawbone. This results in a more natural feel and allows for better eating and speaking functionality. With dental implants, elders can enjoy their favorite foods without worry and speak confidently without the fear of their dentures shifting.
Improved Oral Hygiene
Dental implant seniors often experience improved oral hygiene compared to those with traditional dentures. Implants act like natural teeth and do not require special adhesives or extensive cleaning routines. Regular brushing and flossing are sufficient to keep the implants and surrounding gums healthy. This simplicity in care reduces the risk of oral infections and promotes better overall dental health.
Increased Confidence and Quality of Life
Missing teeth or ill-fitting dentures can lead to self-consciousness and social withdrawal. Dental implants restore a complete, natural-looking smile, boosting self-esteem and encouraging social interaction. Seniors with dental implants often report a higher quality of life, enjoying activities and engagements they might have previously avoided due to dental concerns.
Factors Affecting Older Adults’ Candidacy for Implant Dentistry
Determining whether an older adult is suitable for implant dentistry involves evaluating several critical factors. These considerations ensure that the individual can undergo the procedure safely and achieve successful results. Key factors include:
Overall Health and Medical History
When considering full-mouth dental implants for seniors, evaluating their health and medical history is crucial. Chronic conditions such as diabetes, osteoporosis or autoimmune diseases can affect the healing process after implant surgery. These conditions may slow recovery or increase the risk of complications, so seniors must have these health issues well-managed before undergoing the procedure.
In addition, certain medications, especially those for osteoporosis (such as bisphosphonates), blood thinners and immunosuppressants, can affect bone health and the success of dental implants for seniors. It’s crucial for patients to discuss their complete list of medications with their dentist to evaluate any potential risks and plan accordingly.
Dental Health
The health of the gums is a critical factor in determining whether an older adult is a suitable candidate for dental implants. Periodontal disease, which is common among seniors, can compromise the success of the implants. Healthy gums are necessary for providing a stable foundation for the implants. Therefore, any existing gum disease must be treated before implant dentistry.
Moreover, the quality and quantity of the jawbone are vital considerations for full mouth dental implants for seniors. Bone loss in the jaw, often a result of prolonged tooth loss, can affect the stability of the implants. In some cases, bone grafting may be necessary to build up the jawbone to a level that can effectively support the implants. A thorough examination, including imaging, will help determine if the jawbone is adequate for implant placement.
Lifestyle Factors
Lifestyle choices, especially smoking, have a significant impact on the success of dental implants for seniors. Smoking reduces blood flow to the gums and bone, which hinders the healing process and increases the risk of implant failure. Seniors who smoke are strongly advised to quit smoking before undergoing implant surgery to improve the chances of a successful outcome.
Also, a solid commitment to oral hygiene is essential for the long-term success of implants for seniors. Consistent and proper oral care routines help prevent infections and ensure the health of the implants and surrounding tissues. Seniors considering dental implants must be prepared to maintain diligent oral hygiene practices.
Implant Procedure and Recovery for Older Adults
Undergoing implant dentistry is a significant decision, especially for older adults seeking to restore their dental function and aesthetics. The implant procedure and recovery process for seniors involve carefully planned steps to ensure safety, comfort and successful outcomes.
Here’s what to expect when getting dental implants:
The Consultation and Planning Phase
Discussing Patient’s Goals and Expectations
The journey to receiving full-mouth dental implants for seniors begins with a detailed consultation and planning phase. During this stage, the dentist discusses the patient’s goals and expectations for the procedure. Understanding the desired outcomes helps tailor the treatment plan to meet the specific needs and preferences of the senior patient.
Conducting Necessary Examinations and Tests
Comprehensive examinations and tests assess the patient’s suitability for implants. This includes detailed dental imaging, such as X-rays or CT scans, to evaluate the jawbone’s condition and surrounding structures. These assessments help in planning the precise placement of the implants.
The Surgical Procedure
Anesthesia and Sedation Options
For the surgical placement of implants for seniors, anesthesia and sedation options are carefully considered to ensure comfort and ease during the procedure. Depending on the complexity of the case and the patient’s health status, options range from local anesthesia to general anesthesia or conscious sedation.
The Placement of the Implant
During the surgery, the dental implants are placed into the jawbone. This involves making an incision in the gum, drilling a small hole in the bone and securely placing the implant. The precision of this process is crucial for the stability and longevity of the implants. For full mouth dental implants for seniors, multiple implants may be placed to support a full arch of replacement teeth.
Post-Surgical Healing and Recovery
Potential Risks and Complications
Like any surgical procedure, dental implants carry potential risks and complications. These may include infection, implant failure or issues with the integration of the implant into the jawbone. To minimize complications, seniors must understand these risks and follow their dentist’s post-operative care instructions.
Proper Care and Maintenance of the Implant Site
Proper care and maintenance of the implant site are essential for successful healing. This includes keeping the area clean, avoiding certain foods, and following a prescribed oral hygiene routine. Regular follow-up visits with the dentist are also crucial to monitor the healing process and address any issues promptly.
The Placement of the Prosthesis
Customizing the Tooth or Teeth Replacement
Once the implants have fully integrated with the jawbone, the final step is the prosthesis placement. This involves customizing the tooth or replacing teeth to match the patient’s natural teeth in color, shape, and size. This customization ensures a natural and aesthetically pleasing appearance.
Ensuring Proper Fit and Function
The final prosthesis is carefully adjusted to ensure proper fit and function. This step is critical for the patient’s comfort and ability to chew and speak effectively. Ensuring the correct alignment and fit helps maintain the health of the surrounding teeth and gums, contributing to the long-term success of the implants.
Cost Considerations
The cost of implant dentistry can vary widely based on several factors. These include the number of implants needed, the complexity of the procedure, the type of implants used, and any additional treatments required, such as bone grafting or sinus lifts. The dental professional’s geographic location and experience can also impact the cost. Given these variables, it’s best to discuss your specific needs and potential expenses with a dental professional to understand what to expect financially.

Invest in a Confident Smile at Archpoint Implant Dentistry
Implant dentistry has made great strides in providing older adults with reliable, safe, and comfortable solutions to restore their oral health and confidence. As highlighted in this blog, there is much to consider when deciding upon dental implant treatment for seniors. However, if you’re armed with the correct information and guidance, it can undoubtedly be a transformative experience.
At Archpoint Implant Dentistry, we understand the unique needs and desires of our senior patients. With our team of expert dental professionals and state-of-the-art technology, we’re committed to providing the highest standard of care and making your experience as seamless as possible. We will work closely with you to develop a personalized treatment plan for your oral health needs.
Contact us today for a free consultation.